Risposta immunitaria innata e adattativa
Le cellule mieloidi, come i granulociti, i monociti, le cellule NK e le cellule dendritiche contribuiscono al sistema immunitario innato nel riconoscere gli agenti patogeni e i danni tissutali. Queste cellule si attivano al contatto con microbi e di segnali di danno (PAMPs, DAMPs) innescando una robusta risposta infiammatoria e rilasciando vari mediatori pro-infiammatori come citochine, interferoni (IFNs) e marcatori cellulari specifici. Ciò costituisce la risposta immediata all'infezione, data dal sistema immunitario innato.
L'immunità adattativa, che è necessaria per la risposta a lungo termine, è attivata attraverso la classica interazione MHCI e II/TCR con le cellule dendritiche attivate. Gli interferoni agiscono anche come collegamento chiave tra la risposta immunitaria innata e l'attivazione della risposta immunitaria adattativa.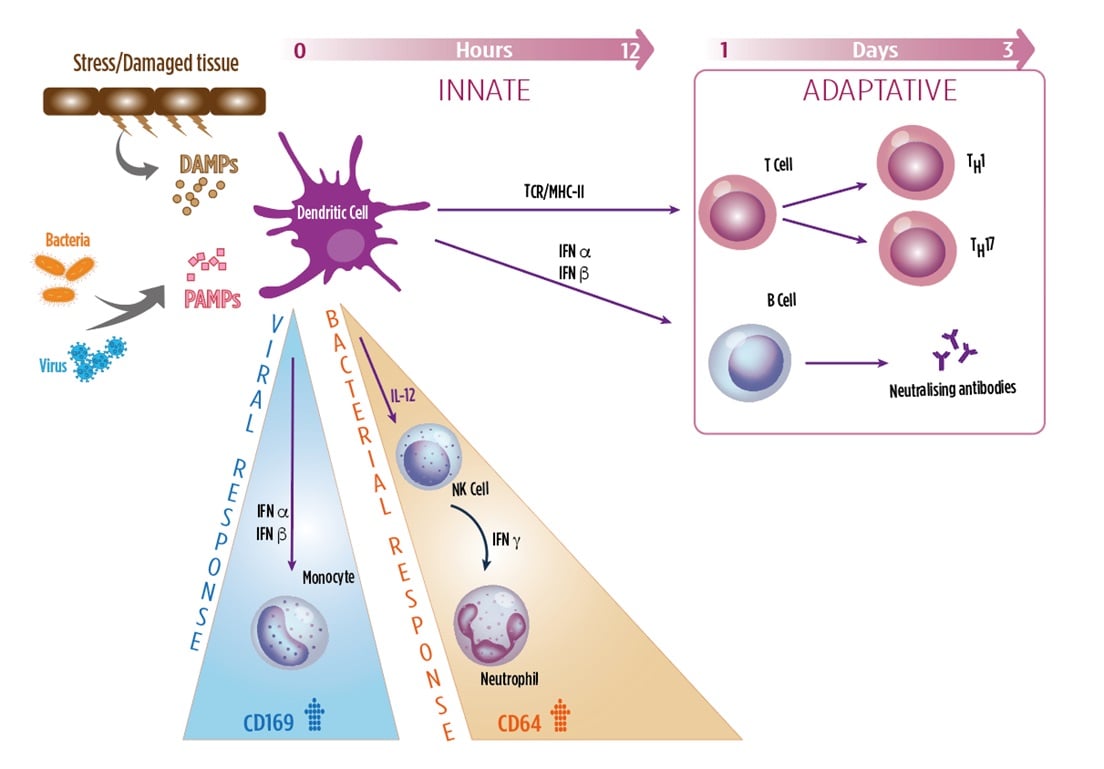
CD64 (FCγ-RI)
- Provide a first line of recognition and defense against infections
- Bacterial infections, leads to release of type II IFN (IFNγ), which strongly induces the expression of CD64 on neutrophils.
CD169 (Siglec-1)
- Adhesion receptor, recognizing sialylated glycoproteins and glycolipids of viral membranes
- Viral infections, leads to release of type I IFNs (IFNα, β), which strongly induces expression of CD169 on monocytes
HLA-DR
- MHC-Class II receptor mainly involved in viral antigen presentation to T cells
- HLA-DR on monocytes is induced immediately after infection, slowly declining with exhaustion.
References:
- Crocker PR. Properties and distribution of a lectin-like hemagglutinin differentially expressed by murine stromal tissue macrophages. J. Exp. Med. 164(6), 1862–1875 (1986).
- Macauley MS, Crocker PR, Paulson JC. Siglec regulation of immune cell function in disease. Nat. Rev. Immunol. 14(10), 653–666 (2014).
- Pino M, Erkizia I, Benet S, et al. HIV-1 immune activation induces Siglec-1 expression and enhances viral trans-infection in blood and tissue myeloid cells. Retrovirology 12(1), 1–15 (2015).
- Kim W-K, McGary CM, Holder GE, et al. Increased Expression of CD169 on Blood Monocytes and Its Regulation by Virus and CD8 T Cells in Macaque Models of HIV Infection and AIDS. AIDS Res. Hum. Retroviruses 31(7), 696–706 (2015).
- Bourgoin P, Biéchelé G, Ait Belkacem I, Morange PE, Malergue F. Role of the interferons in CD64 and CD169 expressions in whole blood: Relevance in the balance between viral- or bacterial-oriented immune responses. Immun Inflamm Dis. 2020;8(1):106-123. doi:10.1002/iid3.289.
- Kipfmueller F, Schneider J, Prusseit J, et al. Role of Neutrophil CD64 Index as a Screening Marker for Late Onset Sepsis in Very Low Birth Weight Infants. PLoS ONE 10(4), 1–15 (2015).
- Selvaraj P, Fifadara N, Nagarajan S, Cimino A, Wang G. Functional Regulation of Human Neutrophil Fc γ Receptors. Immunol. Res. 29(1–3), 219–230 (2004).
- Krensky, A.M. The HLA system, antigen processing and presentation. 1997, Kidney International, suppl. 58, 51, 2-7.
- Lee, J., Dupont, B.O. The HLA system: An introduction. 1990, "The HLA system: A new approach", Springer-Verlag, 1-26.
- Uckun, F.M. Regulation of human B-cell ontogeny. 1990, Blood, 76, 1908-1923.
- Kontny, E., Ryzewska, A. Surface markers on human activated T lymphocytes IV. Comparison of high-affinity E-rosette receptor expression with the expression of other activation markers (receptor for Interleukin 2, MHC class II (antigens). 1990, Archivum Immunologiae et Ther. Experimentalis, 38, 421-431.
- Venet F, Lukaszewicz AC, Payen D, Hotchkiss R, Monneret G. Monitoring the immune response in sepsis: a rational approach to administration of immunoadjuvant therapies. Curr Opin Immunol. 2013;25(4):477-483. doi:10.1016/j.coi.2013.05.006.

